At least 15,000 Tricare beneficiaries lost their health care insurance after delays and fights over data caused problems for Tricare's incoming contractors last year, according to a recent Government Accountability Office report.
In total, about 224,000 beneficiaries were put at risk of losing their insurance, the report said, because beneficiaries' credit cards or other payments could not be shared with the incoming contractors.
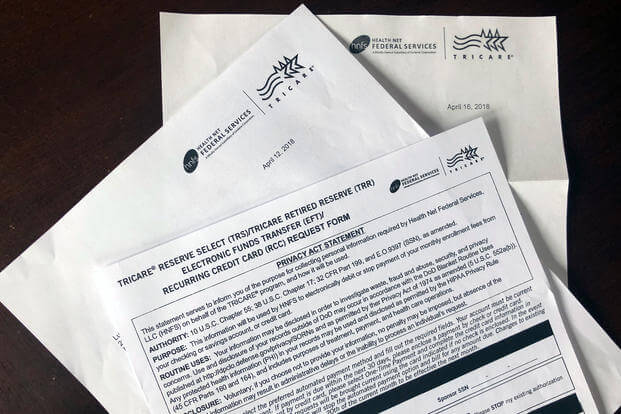
The Defense Health Agency manages Tricare through contracts that change every few years with various private health care insurance companies. The latest contract, called T-2017, is with Health Net Federal Services in the West and Humana Military in the East. They began covering Tricare's 9.5 million beneficiaries on Jan. 1, 2018, and the contracts are set to expire on Dec. 31, 2022.
"According to incoming contractor officials," GAO staff said in the report, "this created additional, unanticipated effort, since they had to contact beneficiaries for this information directly, which diverted transition resources, such as enrollment staff, away from ongoing transition activities."
Related: They Claim They Sent Tricare Warning Letters, But I Never Got Them
The beneficiaries who lost their plans were enrolled in Tricare Reserve Select, Tricare Retired Reserve or Tricare Young Adult, GAO staff reported. This is probably because these plans require a recurring payment.
Tricare users in those plans were first told to update their information by late December 2017 because the payment information could not be shared. But many of those who did so ultimately had their information lost anyway thanks to an enrollment blackout put in place over that month.
The Defense Health Agency, which contracts Tricare management to private companies, granted a 150-day grace period for premium payments.
This report on the DHA's latest round of health care insurance contracts also found transition issues that went beyond the trouble caused by one-time events, like consolidating the Tricare regions from three to two and issuing new policies relating to Tricare Standard after it was renamed Tricare Select.
"A smooth transition of health care delivery between outgoing and incoming managed care support contractors helps ensure continuity of care for Tricare beneficiaries," the report states. "While the implementation of a new benefit option during the T-2017 contract transition was a one-time occurrence, our review highlighted weaknesses in DHA's transition guidance and oversight that could pose challenges to future contract transitions."
The GAO recommended that DHA better define its data-sharing requirements and increase response time for when contractors disagree on which data to share.
In one case, the GAO report found the DHA took almost four and a half months to decide how much historical and authorization data the new Tricare West contractor could request.
This negatively impacted Health Net Federal Services' ability to resolve beneficiaries' questions about referrals or help clinics address customer referral inquiries, GAO staff said, damaging its relationship with both.
In the end, the DHA rejected HNFS's request for the older data because "the outgoing contractor would not have enough time to provide it by the start of health care delivery on January 1, 2018."
Meanwhile, the GAO noted that without access to "more detailed historical information from the claims notes, there were instances in which they were unable to adjust payment determinations for certain claims paid prior to transition, which resulted in provider and beneficiary dissatisfaction."
Related: Bad Provider Listings, Slow Claims Problems Continue for Tricare
Issues previously reported by Military.com were also described in the report. The GAO found both contractors' directories were less than 77% accurate as of June 2019. GAO staff said both contractors countered that the 95% accuracy standard is too high.
It further found the East region contractor, Humana Military, needs to improve the accuracy of its claims processing and has only recently reached the DHA's timeliness standard.
The Defense Department agreed with the GAO's findings. The DHA is naming specific types of data to be shared in its transition guidance, and its staff is creating a "formal process" to ensure all questions are answered in a timely manner.
-- Dorothy Mills-Gregg can be reached at dorothy.mills-gregg@military.com. Follow her on Twitter at @DMillsGregg.
Read More: US Military Makes Bold Statement in First-of-its-Kind Exercise with India